Artificial Cervical Discs – How do they work?
Disc replacement surgery represents a powerful, well-established tool for treating disc herniations and cervical disc disease in selected patients. That’s good news for patients who have persistent pain and dysfunction due to neck pain, who still want to avoid a spine fusion if they can.
So, what’s the role of Disc Replacement Surgery in 2022? There’s good news and bad news…
So, what’s the role of Disc Replacement Surgery in 2022? There’s good news and bad news…
Good news!! Most patients with neck pain recover without surgery: 80-90% will get better, and back to normal activity with physical therapy, anti-inflammatory meds, rest, activity modifications, chiropractic manipulation…or, in some cases with nothing but time and TLC!
Bad News!! About 10-15% of patients with a serious neck problem will eventually need surgery. They’ll need an operation to relieve persistent arm pain due to a herniated disc, arm pain and weakness due to nerve root compression caused by disc degeneration, or surgery to treat instability or deformity.
When persistent neck and arm pain are annoying, we can treat those well with a number of different non-operative strategies – physical therapy, manipulation, oral medications, or injection therapy. But when pain is bad enough that it interferes with daily function, employment, fitness, sleep…surgery starts to make sense.
Who needs spine surgery?
We consider surgery for patients who have structural neck pain problems, such as disc degeneration, instability, deformity or more serious issues such as fracture, infection, or tumor. We also depend on surgery as a reliable solution for many causes of arm pain or weakness (radiculopathy) including disc herniation, cervical stenosis, or segmental instability.
Bad News!! About 10-15% of patients with a serious neck problem will eventually need surgery. They’ll need an operation to relieve persistent arm pain due to a herniated disc, arm pain and weakness due to nerve root compression caused by disc degeneration, or surgery to treat instability or deformity.
When persistent neck and arm pain are annoying, we can treat those well with a number of different non-operative strategies – physical therapy, manipulation, oral medications, or injection therapy. But when pain is bad enough that it interferes with daily function, employment, fitness, sleep…surgery starts to make sense.
Who needs spine surgery?
We consider surgery for patients who have structural neck pain problems, such as disc degeneration, instability, deformity or more serious issues such as fracture, infection, or tumor. We also depend on surgery as a reliable solution for many causes of arm pain or weakness (radiculopathy) including disc herniation, cervical stenosis, or segmental instability.
Not every type of operation works for each of these problems, though, and each has its strengths and its drawbacks. Disc replacement surgery is an excellent treatment for disc herniations and disc degeneration, but it is not a treatment for spinal instability or deformity, and not at all useful for treating tumors, infections, or fractures and dislocations of the cervical spine. Cervical fusion remains the very best solution for each of those problems.
For those patients who suffer neck and arm pain due to disc degeneration or herniation, disc replacement – or cervical arthroplasty – is an important option.
For those patients who suffer neck and arm pain due to disc degeneration or herniation, disc replacement – or cervical arthroplasty – is an important option.
Who needs disc surgery?
Degeneration of the Intervertebral Disc causes changes in disc, which sits between each of the vertebral bodies and acts as a shock absorber and slightly flexible joint. As we age, the molecular components of the disc change, resulting in a loss of water-holding capacity, and a progressive loss of elasticity and compressive strength – the disc becomes a less successful shock-absorber.
On x-rays we see:
Bone spurs (osteophytes) form around the facet joints and edges of the discs themselves
Disc damage that causes bulging and herniation
Loss of normal mechanical stability, loss of disc height, and loss of normal neck posture
We can even see structural deformity
These changes go along with the symptoms we see:
Axial neck pain – pain in the muscles and ligaments of the neck, stiffness, shoulder and back pain;
Referred pain - symptoms over the trapezius, rhomboids, and shoulder blades
Tension myositis - muscular pain, often causing headaches; and
Radicular pain - pain in the spinal nerve distribution causing pain down the arm and into the hand and fingers
Radicular arm pain is the symptom most commonly requiring surgery.
When these symptoms are severe, interfering with fitness health, and normal rest, and when they fail to improve after a good trial of non-operative care, that’s when we consider surgery.
The general rules for choosing surgery for a patient start with the symptoms:
Degeneration of the Intervertebral Disc causes changes in disc, which sits between each of the vertebral bodies and acts as a shock absorber and slightly flexible joint. As we age, the molecular components of the disc change, resulting in a loss of water-holding capacity, and a progressive loss of elasticity and compressive strength – the disc becomes a less successful shock-absorber.
On x-rays we see:
Bone spurs (osteophytes) form around the facet joints and edges of the discs themselves
Disc damage that causes bulging and herniation
Loss of normal mechanical stability, loss of disc height, and loss of normal neck posture
We can even see structural deformity
These changes go along with the symptoms we see:
Axial neck pain – pain in the muscles and ligaments of the neck, stiffness, shoulder and back pain;
Referred pain - symptoms over the trapezius, rhomboids, and shoulder blades
Tension myositis - muscular pain, often causing headaches; and
Radicular pain - pain in the spinal nerve distribution causing pain down the arm and into the hand and fingers
Radicular arm pain is the symptom most commonly requiring surgery.
When these symptoms are severe, interfering with fitness health, and normal rest, and when they fail to improve after a good trial of non-operative care, that’s when we consider surgery.
The general rules for choosing surgery for a patient start with the symptoms:
- Arm pain not responsive to a good trial (3 months) of conservative therapy
- Any progressive neurological deficit
- A persistent neurological deficit with persistent radicular pain
- A surgically correctable lesion has been confirmed on imaging studies
- Any progressive instability or deformity
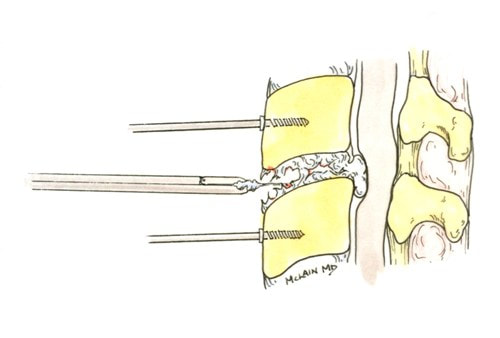
The traditional treatment for cervical disc herniation is an anterior cervical discectomy (surgical removal of the disc) and fusion (ACDF). That’s a surgery through the front of the neck, through which the disc is removed all the way back to the spinal canal.
But, why fuse the spine after you get the disc out?
The interbody fusion (placing a cage or bone between the endplates of the adjacent vertebrae) restores intervertebral and foraminal height, immobilizes the painful segment, and provides permanent stability.
But it eliminates motion at the treated level and increases stresses in the adjacent levels above or below, and that can lead to breakdown at that adjacent level, (adjacent level degeneration) sometimes just a year or two after the initial surgery.
What does the Artificial Disc do that’s different?
The cervical disc arthroplasty or disc replacement is intended for the patient who would otherwise need a fusion.
But, why fuse the spine after you get the disc out?
The interbody fusion (placing a cage or bone between the endplates of the adjacent vertebrae) restores intervertebral and foraminal height, immobilizes the painful segment, and provides permanent stability.
But it eliminates motion at the treated level and increases stresses in the adjacent levels above or below, and that can lead to breakdown at that adjacent level, (adjacent level degeneration) sometimes just a year or two after the initial surgery.
What does the Artificial Disc do that’s different?
The cervical disc arthroplasty or disc replacement is intended for the patient who would otherwise need a fusion.
The approach for the disc arthroplasty, and the removal of the damaged or herniated disc is exactly the same as in the traditional ACDF procedure, but instead of placing bone or a fusion cage in the empty disc space, disc replacement surgery replaces the damaged intervertebral disc with an artificial device that restores disc height and alignment and preserves the motion of the original disc. This allows the treated spinal level to move more naturally, reducing the risk of adjacent level degeneration down the road.
Who is a good candidate for a disc replacement?
Who is a good candidate for a disc replacement?
- Patients with at least 6-12 weeks of persistent pain, that hasn’t responded to a good trial of conservative therapy
- Patients with radicular pain or weakness causing serious functional impairment
- Patients whose surgical problem is limited to one or two disc-levels
- Patients with disc disease at one or two-levels between the C2-3 to C6-7 levels
- Patients with good bone quality and fitness
- Patients who still demonstrate residual motion at the treatment levels on flexion and extension x-rays.
Where will disc arthroplasty work well?
Success has been unequivocally demonstrated in the well-maintained but painful disc, in the young and active patients.
What about older patients? If patients are reasonably fit, and bone quality is good, age isn’t a big factor! Studies of disc replacement have included patients up to age 69, and my experience with patients older than this suggests disc replacements are just as successful, and better tolerated than the traditional fusion.
What about activity level? Patients that are athletic or hard working can depend on disc replacements to hold up to high demands – they are not fragile.
What about smokers? Well, first off – stop! It’s not good for you. However, smoking does not affect the outcome of disc replacement surgery the way it can a fusion, so disc replacement is probably a better choice for you too.
Here's the caveat:
With that in mind, cervical disc arthroplasty offers an attractive and valuable option for most patients otherwise indicated for cervical fusion to treat their neck and arm pain. If you’ve been offered a fusion surgery, ask your surgeon if you’re a candidate for disc replacement!
As always, I hope you find this discussion interesting and useful. If you have other questions that I can answer for you, please comment below. And feel free to like and share this content with others that might find it beneficial!
Success has been unequivocally demonstrated in the well-maintained but painful disc, in the young and active patients.
What about older patients? If patients are reasonably fit, and bone quality is good, age isn’t a big factor! Studies of disc replacement have included patients up to age 69, and my experience with patients older than this suggests disc replacements are just as successful, and better tolerated than the traditional fusion.
What about activity level? Patients that are athletic or hard working can depend on disc replacements to hold up to high demands – they are not fragile.
What about smokers? Well, first off – stop! It’s not good for you. However, smoking does not affect the outcome of disc replacement surgery the way it can a fusion, so disc replacement is probably a better choice for you too.
Here's the caveat:
- Any recommendation of surgical treatment should be about selecting the best option for each individual patient, considering their particular symptoms and challenges, and their age, health, and demands.
- The surgeon’s job is to offer the treatment that carries the highest likelihood for treatment success and the lowest risk of serious complications, again considering each patient’s particular circumstance.
With that in mind, cervical disc arthroplasty offers an attractive and valuable option for most patients otherwise indicated for cervical fusion to treat their neck and arm pain. If you’ve been offered a fusion surgery, ask your surgeon if you’re a candidate for disc replacement!
As always, I hope you find this discussion interesting and useful. If you have other questions that I can answer for you, please comment below. And feel free to like and share this content with others that might find it beneficial!