Back Pain and Spine Surgery: Things You Should Know about Spinal Fusion
Patients with spinal problems that result from “wear and tear” of the spine – disc degeneration - present one of three ways.
Most patients experience back pain as their primary symptom, sometimes severe and disabling, sometimes dull and constant and mostly aggravating. Less frequently, but still pretty often, patients experience leg pain, a burning or tingling sensation running down the thigh or calf towards the foot, sometimes associated with muscular weakness. Finally, many patients are unlucky enough to suffer with a combination of both back and leg pain.
Which of these pain patterns a patient has determines more about his or her subsequent evaluation, treatment, and prognosis for recovery than does any other aspect of evaluation or care. So, the first and often most important question your doctor will ask is, “Where does it hurt?”.
The Causes of Back Pain:
The sensation of pain that any individual experiences is determined by the nature, or cause, of the pain, and the location of the pain generator – the actual structure or tissue that is generating the pain signals.
Pain is produced when:
The kind of back pain that most people experience is the result of several things happening all at once. Or more likely, a number of things piling up over the years until they all start affecting you all at once!
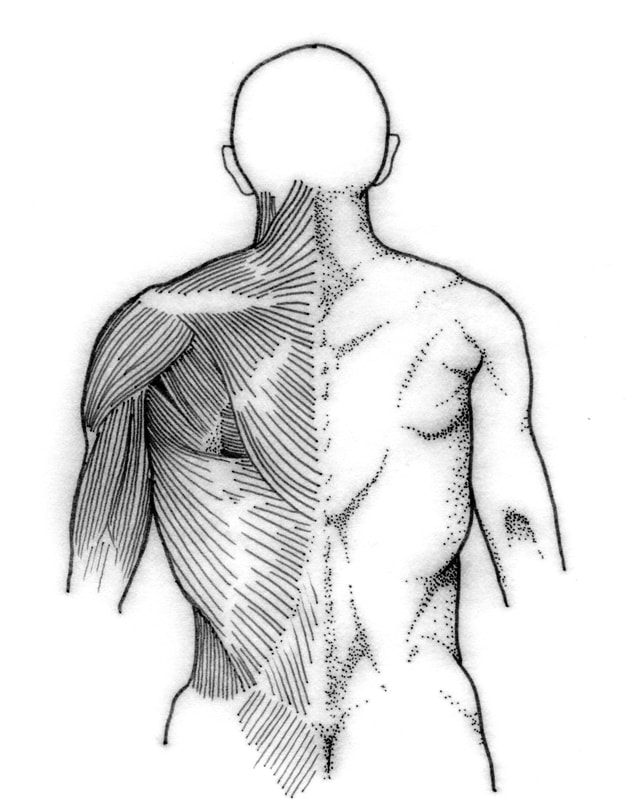
An underlying level of “wear and tear” may have been building up for years. The disc may have lost some of its water content, or the facet joints may have become arthritic. A direct injury to the back could result in a fracture or ligament injury. On top of these issues, the back muscles have gotten out of shape and flabby, and can no longer do their required job without becoming painful and going into spasm. And that leads to all of the other muscles of the buttocks, hips, and back to become de-conditioned and easily irritable.
The sensation of pain that any individual experiences is determined by the nature, or cause, of the pain, and the location of the pain generator – the actual structure or tissue that is generating the pain signals.
Pain is produced when:
- normal tissue is fractured, torn, or crushed
- any tissue with nerve endings is exposed to prolonged or excessive mechanical pressure
- blood supply is cut off to muscle or nerve
- a nerve is directly compressed or irritated
- abnormal or excessive motion stretches or pinches connective tissues
- nerve endings are exposed to chemicals that irritate and inflame them
The kind of back pain that most people experience is the result of several things happening all at once. Or more likely, a number of things piling up over the years until they all start affecting you all at once!
An underlying level of “wear and tear” may have been building up for years. The disc may have lost some of its water content, or the facet joints may have become arthritic. A direct injury to the back could result in a fracture or ligament injury. On top of these issues, the back muscles have gotten out of shape and flabby, and can no longer do their required job without becoming painful and going into spasm. And that leads to all of the other muscles of the buttocks, hips, and back to become de-conditioned and easily irritable.
With all of these things going on, no wonder your back hurts!
Now imagine trying to provide one simple treatment that can fix all of those things – and more – at the same time. This is why back pain care requires a multidisciplinary approach (calling on health care providers with a variety of skills and interests) and lots of patience.
Back Pain
Now imagine trying to provide one simple treatment that can fix all of those things – and more – at the same time. This is why back pain care requires a multidisciplinary approach (calling on health care providers with a variety of skills and interests) and lots of patience.
Back Pain
80 – 90% of all back pain is idiopathic – meaning that we don’t really know what exactly is causing it. We call it mechanical back pain if it’s made worse by activity or motion, but that doesn’t always get us closer to understanding the source of the pain. And that’s because there usually isn’t just one source.
Back pain that persists long enough to warrant a specific evaluation usually has more than one contributing factor:
If the pain came on suddenly, after an acute injury, then it’s likely that there has been an acute injury to the muscles and ligaments of the back. But there is also an immediate release of inflammatory substances into the tissue that causes swelling and pain. These substances make the local nerve endings more sensitive to minor irritations. If there is a fracture and bone is disrupted, then a hematoma forms which exerts pressure on the surrounding tissues.
If the pain came on insidiously over time, or has become chronic, then degenerative processes have probably affected the intervertebral disc and the facet joints, and may do so at several adjacent levels. Inflammation plays a role here as well, and back muscle fatigue and spasm are common.
Back pain that persists long enough to warrant a specific evaluation usually has more than one contributing factor:
If the pain came on suddenly, after an acute injury, then it’s likely that there has been an acute injury to the muscles and ligaments of the back. But there is also an immediate release of inflammatory substances into the tissue that causes swelling and pain. These substances make the local nerve endings more sensitive to minor irritations. If there is a fracture and bone is disrupted, then a hematoma forms which exerts pressure on the surrounding tissues.
If the pain came on insidiously over time, or has become chronic, then degenerative processes have probably affected the intervertebral disc and the facet joints, and may do so at several adjacent levels. Inflammation plays a role here as well, and back muscle fatigue and spasm are common.
In either case, conservative therapy is the first line of treatment, and it has a lot to offer.
The vast majority of acute injuries will resolve and recover on their own, and physical therapy and pain management can help speed that process. Except in severe injuries such as major fractures or ligamentous disruptions, surgery for these acute injuries provides no benefit over non-operative care, only serving to increase risk and local tissue trauma.
Back Pain in Acute Strain or Injury is produced by:
Even when acute back pain lingers or progresses, sorting out exactly which tissue is causing the pain, or even which level of the spine is painful, can be very difficult. There is no test or imaging study that shows "pain", and the physician must be careful not to attribute poorly localized or diffuse symptoms to a single structure just because it looks odd or diseased on radiographs. That’s because:
MRI overestimates back disease: 30% or more of normal, middle aged adults, and 60 – 70% of normal, asymptomatic, older adults (people with no back pain at all) have clearly abnormal MRI studies – with disc degeneration, herniations, facet arthritis, and or stenosis.
And when degeneration affects multiple levels of the spine, it’s not only hard to sort out which level is the primary pain generator, it’s probably true that every level is at least a little bit painful, and that all are contributing to pain and poor function. Operating on multiple levels of the spine can cause more harm than good, so sorting out the primary source of pain is crucial to a successful operation. In the same sense, if you can’t locate a primary pain generator, or if all of the spinal levels are equally symptomatic, then surgical fusion is not likely to help, and probably shouldn’t be attempted without more information.
Although physical therapy can’t reverse the aging process, it can improve function and mobility. Surgery, on the other hand, adds further trauma to the situation without reliably reducing the symptoms of myofascial (muscle, tendons, and ligament) back pain.
Unless back pain symptoms are well localized, and clearly associated with signs of structural instability, deformity, or disc injury, surgical fusion cannot reliably improve the situation.
If instability does exist, however, fusion can provide significant improvement.
The vast majority of acute injuries will resolve and recover on their own, and physical therapy and pain management can help speed that process. Except in severe injuries such as major fractures or ligamentous disruptions, surgery for these acute injuries provides no benefit over non-operative care, only serving to increase risk and local tissue trauma.
Back Pain in Acute Strain or Injury is produced by:
- Any of the back muscles overlying or near the area of injury or irritation
- The structures of and around the facet joints
- The disc and its accompanying ligaments, the anterior and posterior longitudinal ligaments
- The neural elements within the thecal sac and the sack itself
- The nerve roots as they leave the thecal sac and exit the spinal canal
- The bones of the anterior and posterior elements: lamina, processes, pedicles, and the vertebral body
Even when acute back pain lingers or progresses, sorting out exactly which tissue is causing the pain, or even which level of the spine is painful, can be very difficult. There is no test or imaging study that shows "pain", and the physician must be careful not to attribute poorly localized or diffuse symptoms to a single structure just because it looks odd or diseased on radiographs. That’s because:
MRI overestimates back disease: 30% or more of normal, middle aged adults, and 60 – 70% of normal, asymptomatic, older adults (people with no back pain at all) have clearly abnormal MRI studies – with disc degeneration, herniations, facet arthritis, and or stenosis.
And when degeneration affects multiple levels of the spine, it’s not only hard to sort out which level is the primary pain generator, it’s probably true that every level is at least a little bit painful, and that all are contributing to pain and poor function. Operating on multiple levels of the spine can cause more harm than good, so sorting out the primary source of pain is crucial to a successful operation. In the same sense, if you can’t locate a primary pain generator, or if all of the spinal levels are equally symptomatic, then surgical fusion is not likely to help, and probably shouldn’t be attempted without more information.
Although physical therapy can’t reverse the aging process, it can improve function and mobility. Surgery, on the other hand, adds further trauma to the situation without reliably reducing the symptoms of myofascial (muscle, tendons, and ligament) back pain.
Unless back pain symptoms are well localized, and clearly associated with signs of structural instability, deformity, or disc injury, surgical fusion cannot reliably improve the situation.
If instability does exist, however, fusion can provide significant improvement.
Surgical Treatment for Back Pain:
There are a number of causes of back pain that can be helped by surgery, but almost none that can be cured outright, or without some form of rehabilitation and conditioning program after surgery.
Fusion, also called arthrodesis, is the cornerstone to surgical treatment of back pain. A posterolateral lumbar fusion is the key part of the surgical management of many spinal disorders. This utilitarian surgical procedure has been used to treat thoracolumbar and lumbar instability caused by fractures, disc degeneration, or spondylolisthesis. It has been used successfully in the treatment of lumbar disc disease and discogenic pain. Additionally, posterolateral arthrodesis may be used to reconstruct the spine when more destructive processes, such as tumors or spinal infections, disrupt the spinal column.
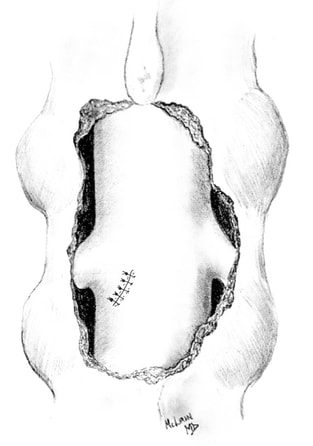
The posterolateral fusion is the most commonly performed spinal fusion. It consists of a surgical exposure of the dorsal elements of the involved spinal segments, followed by preparation of the "fusion bed", and placement of a bone graft. In essence, the surgeon tries to confuse the body’s normal repair process: by removing the outer shell of bone – the cortex – and exposing the inner portion – the cancellous bone – the body is convinced that the spinal elements have been fractured. The normal healing response is triggered and the decorticated bone segments are incorporated into a single segment as the body seeks to heal the “fractured” parts.
The success of the fusion depends on the biological preparation of the fusion bed - the area where new bone is going to form. Blood supply to the fusion mass comes from the decorticated transverse processes and the surrounding walls of muscle tissue. Also, the maximal area possible must be decorticated as fusion rates may be related to increased surface area. Finally, new bone material needs to be placed in the bed - sometimes from allograft (other patients donated, sterilized bone), or autograft (your own bone) taken from the spinal segments being decompressed or transplanted from the iliac crest. Autograft bone increases the likelihood of fusion success, but harvesting it can take time and cause additional pain.
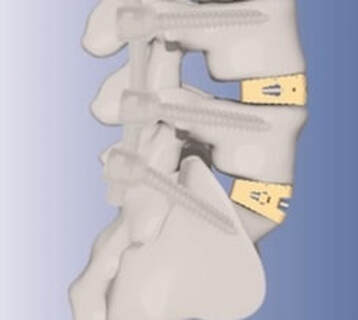
Failure of the fusion to occur can cause treatment failure. Nonunion occurs in 5-35% of un-instrumented spinal fusions - fusions carried out by simply placing bone graft into the fusion bed. Spinal instrumentation (rods and screws) has reduced the failure rate to 5-15%. Spinal instrumentation allows patients to get up quicker and to mobilize without a cumbersome brace.
Although a variety of novel internal fixation devices have been used since the early 1900’s, pedicle screws, used with fixation rods, have significantly improved the treatment of spinal disorders and have been incorporated into most current implant systems. The majority of posterolateral fusions performed today are stabilized with a pedicle screw and rod construct.
There are a number of causes of back pain that can be helped by surgery, but almost none that can be cured outright, or without some form of rehabilitation and conditioning program after surgery.
Fusion, also called arthrodesis, is the cornerstone to surgical treatment of back pain. A posterolateral lumbar fusion is the key part of the surgical management of many spinal disorders. This utilitarian surgical procedure has been used to treat thoracolumbar and lumbar instability caused by fractures, disc degeneration, or spondylolisthesis. It has been used successfully in the treatment of lumbar disc disease and discogenic pain. Additionally, posterolateral arthrodesis may be used to reconstruct the spine when more destructive processes, such as tumors or spinal infections, disrupt the spinal column.
The posterolateral fusion is the most commonly performed spinal fusion. It consists of a surgical exposure of the dorsal elements of the involved spinal segments, followed by preparation of the "fusion bed", and placement of a bone graft. In essence, the surgeon tries to confuse the body’s normal repair process: by removing the outer shell of bone – the cortex – and exposing the inner portion – the cancellous bone – the body is convinced that the spinal elements have been fractured. The normal healing response is triggered and the decorticated bone segments are incorporated into a single segment as the body seeks to heal the “fractured” parts.
The success of the fusion depends on the biological preparation of the fusion bed - the area where new bone is going to form. Blood supply to the fusion mass comes from the decorticated transverse processes and the surrounding walls of muscle tissue. Also, the maximal area possible must be decorticated as fusion rates may be related to increased surface area. Finally, new bone material needs to be placed in the bed - sometimes from allograft (other patients donated, sterilized bone), or autograft (your own bone) taken from the spinal segments being decompressed or transplanted from the iliac crest. Autograft bone increases the likelihood of fusion success, but harvesting it can take time and cause additional pain.
Failure of the fusion to occur can cause treatment failure. Nonunion occurs in 5-35% of un-instrumented spinal fusions - fusions carried out by simply placing bone graft into the fusion bed. Spinal instrumentation (rods and screws) has reduced the failure rate to 5-15%. Spinal instrumentation allows patients to get up quicker and to mobilize without a cumbersome brace.
Although a variety of novel internal fixation devices have been used since the early 1900’s, pedicle screws, used with fixation rods, have significantly improved the treatment of spinal disorders and have been incorporated into most current implant systems. The majority of posterolateral fusions performed today are stabilized with a pedicle screw and rod construct.
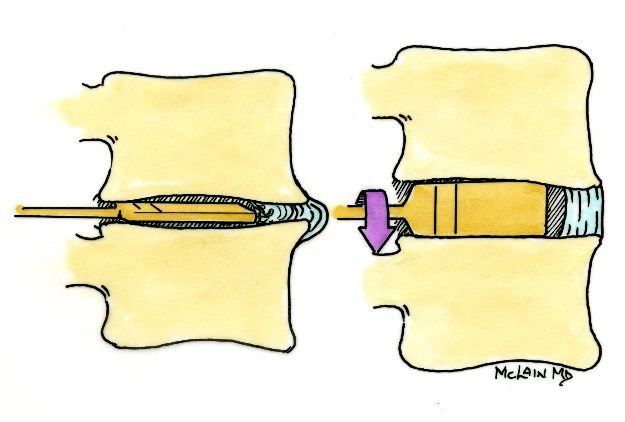
A second option for fusion, particularly useful for degenerative disease at the lowest lumbar levels, is an anterior lumbar interbody fusion, or ALIF. This procedure approaches the spine through the abdomen, avoiding the nerve roots and spinal canal all together.
From the anterior approach the disc can be removed entirely, and the broad surfaces of the vertebral endplates prepared for fusion. A variety of cages and graft materials are available for placement into the disc space. In addition to enhancing the likelihood of fusion, these devices are designed to restore the height and alignment of the diseased spinal segment.
Most cages are designed to be filled with bone graft, to enhance the fusion process. The majority of these devices are intended to be used with supplemental spinal instrumentation, usually posterior screws and rods, placed at a second operation, but many now incorporate an interbody fixation strategy that locks them in place without any need for additional surgery.
From the anterior approach the disc can be removed entirely, and the broad surfaces of the vertebral endplates prepared for fusion. A variety of cages and graft materials are available for placement into the disc space. In addition to enhancing the likelihood of fusion, these devices are designed to restore the height and alignment of the diseased spinal segment.
Most cages are designed to be filled with bone graft, to enhance the fusion process. The majority of these devices are intended to be used with supplemental spinal instrumentation, usually posterior screws and rods, placed at a second operation, but many now incorporate an interbody fixation strategy that locks them in place without any need for additional surgery.
A third approach to lumbar fusion combines the principles of the posterolateral and anterior interbody fusions to give the highest likelihood of a solid fusion and a stable spine. These procedures are often referred to as “360 degree” fusions because they address the spine from both front and back. There are three ways to carry out a 360 fusion.
First, the most traditional way of performing a 360 fusion is to carry out a direct ALIF procedure using a cage or spacer, followed by a traditional posterolateral fusion with instrumentation. Fusion rates are high and success is quite good in well selected patients. This is a big operation to go through, but the spine is stable at the end of surgery and patients can begin getting out of bed very quickly after surgery. Newer, minimally invasive techniques now allow surgeons to perform both aspects of the 360 fusion through small, minimally invasive approaches, resulting in less muscle trauma and incisional pain than seen with traditional techniques
First, the most traditional way of performing a 360 fusion is to carry out a direct ALIF procedure using a cage or spacer, followed by a traditional posterolateral fusion with instrumentation. Fusion rates are high and success is quite good in well selected patients. This is a big operation to go through, but the spine is stable at the end of surgery and patients can begin getting out of bed very quickly after surgery. Newer, minimally invasive techniques now allow surgeons to perform both aspects of the 360 fusion through small, minimally invasive approaches, resulting in less muscle trauma and incisional pain than seen with traditional techniques
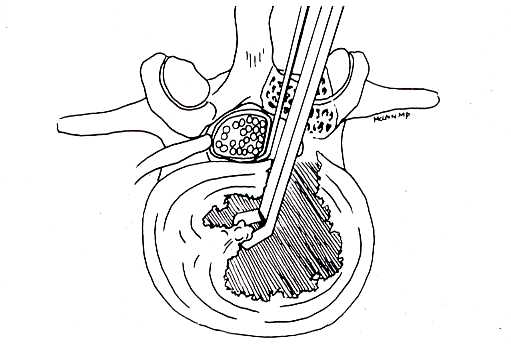
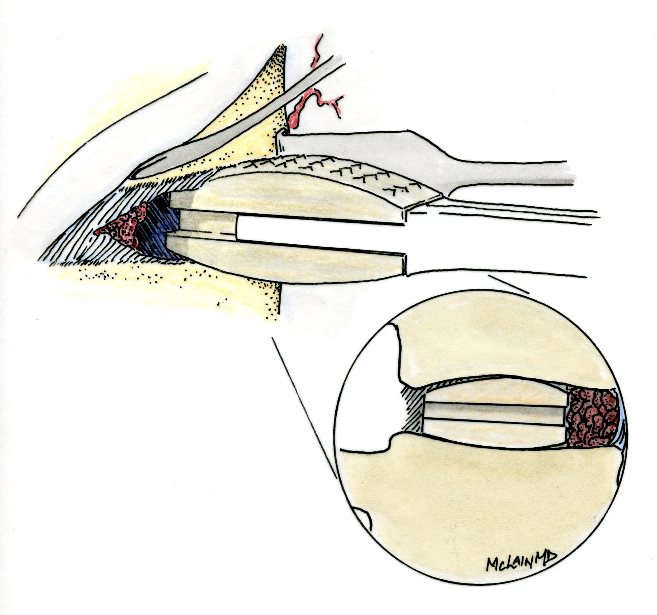
The second option is performed through a single posterior approach - often called a "TLIF" (Transforaminal Lumbar Interbody Fusion procedure - obtaining a fusion of the interbody space through the posterior surgical approach. In this approach the surgeon performs all of the surgery from a posterior approach, frequently taking away all of the overlying bone at the operative level through a laminectomy technique.
Once the spinal canal is open, the nerves are moved out of the way and the surgeon removes all of the affected disc material from behind, in similar fashion to a discectomy.
Once the spinal canal is open, the nerves are moved out of the way and the surgeon removes all of the affected disc material from behind, in similar fashion to a discectomy.
The "disc space" is then packed with bone and a spacer, and the posterior elements fused and instrumented with pedicle screws. This accomplishes the 360 fusion all from the single posterior approach, but the procedure must be carried out with meticulous technique to avoid irritating or injuring the nerves
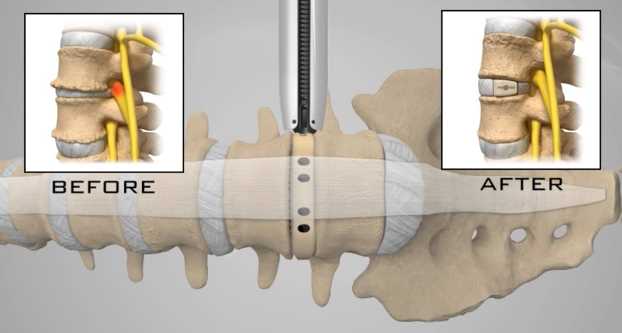
The third option is carried out as a minimally invasive approach through the flank, getting at the disc space from the side, behind the abdominal contents, and either fixing the segment in place with a lateral plate or screws, or reinforcing the fusion with screws delivered from behind. This "XLIF" or "DLIF" approach is suitable for fusions from the L4-L5 level to the lower thoracic spine, but can't be used at the Lumbosacral level.
Patients who are good candidates for fusion include those with radiographically proven segmental instability (excessive motion) secondary to disc degeneration, degenerative spondylolisthesis, degenerative scoliosis, post-discectomy degeneration, or instability caused by previous spinal procedures such as laminectomy or facet joint removal. Other universally accepted indications for lumbar fusion include persistent back and leg pain in the adult related to isthmic spondylolisthesis, adult scoliosis, failed prior surgery, tumor, trauma and infection. There is good evidence that patients with severe back pain due to these conditions will benefit, often dramatically, from a well performed spinal fusion.
There are a number of factors which may have a negative impact on the success of a spinal fusion surgery. These include:
There is one area of spinal disease that is not so clear-cut when it comes to either diagnosis or surgical care. There is currently no area in lumbar spine surgery more controversial than fusion for "discogenic" back pain. Discogenic pain is pain caused by degeneration or disruption of the disc itself, often with no apparent mechanical instability. Whereas fusion for instability is thought to reduce pain by stopping abnormal and painful motion, surgery for discogenic pain is thought to work by relieving the disc of its normal loads and stresses, and by removing the painful disc itself. Despite the difficulty of accurately and reproducibly diagnosing pain caused directly by the damaged disc, many authors have reported successful outcomes in properly selected patients treated with isolated fusions for focal, activity related back pain caused by deteriorating discs.
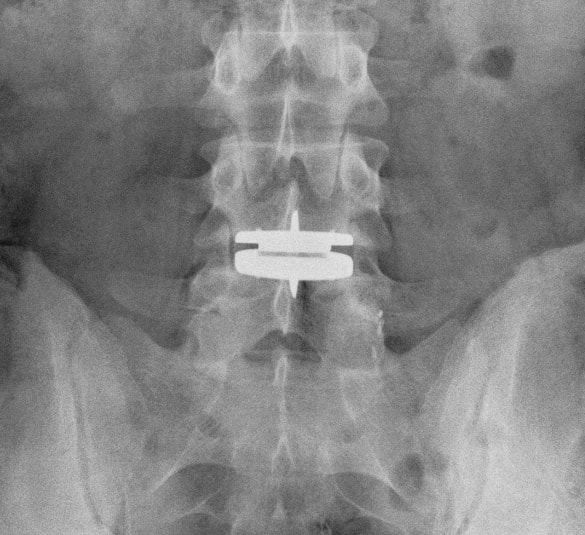
While fusion for discogenic pain has proven successful in reducing pain and improving function and activity levels in well selected patients, another option has become available which may achieve the same result without resorting to fusion. Disc arthroplasty, or artificial disc replacement, has been used in Europe for nearly two decades, with steadily improving results with each new design. Current designs have been under investigation in the United States over the last few years, with very promising results. In 2004, the Food and Drug Administration (FDA) approved the first artificial disc for general use in the treatment of single-level degenerative disc disease and discogenic pain.
Disc arthroplasty is carried out through an incision similar to the one used for anterior interbody fusion. The exposure to the disc is carried out by a surgeon well experienced in anterior spine surgery. The disc – either L4-L5, or L5 –S1 – is almost completely removed, with care taken to remove all the disc material back to the posterior rim of the vertebral body. Once the disc space is meticulously prepared, a properly sized implant, consisting of plates that fit the vertebral endplates and a polyethylene spacer that permits a limited degree of motion, is inserted and carefully embedded into the bone
There are a number of factors which may have a negative impact on the success of a spinal fusion surgery. These include:
- a lack of focal, well defined symptoms of leg pain or back pain,
- advancing age with poor bone quality and poor fitness,
- a history of previous low back surgery,
- increasing number of vertebral levels to be fused,
- diabetes, and – importantly -
- tobacco use.
There is one area of spinal disease that is not so clear-cut when it comes to either diagnosis or surgical care. There is currently no area in lumbar spine surgery more controversial than fusion for "discogenic" back pain. Discogenic pain is pain caused by degeneration or disruption of the disc itself, often with no apparent mechanical instability. Whereas fusion for instability is thought to reduce pain by stopping abnormal and painful motion, surgery for discogenic pain is thought to work by relieving the disc of its normal loads and stresses, and by removing the painful disc itself. Despite the difficulty of accurately and reproducibly diagnosing pain caused directly by the damaged disc, many authors have reported successful outcomes in properly selected patients treated with isolated fusions for focal, activity related back pain caused by deteriorating discs.
While fusion for discogenic pain has proven successful in reducing pain and improving function and activity levels in well selected patients, another option has become available which may achieve the same result without resorting to fusion. Disc arthroplasty, or artificial disc replacement, has been used in Europe for nearly two decades, with steadily improving results with each new design. Current designs have been under investigation in the United States over the last few years, with very promising results. In 2004, the Food and Drug Administration (FDA) approved the first artificial disc for general use in the treatment of single-level degenerative disc disease and discogenic pain.
Disc arthroplasty is carried out through an incision similar to the one used for anterior interbody fusion. The exposure to the disc is carried out by a surgeon well experienced in anterior spine surgery. The disc – either L4-L5, or L5 –S1 – is almost completely removed, with care taken to remove all the disc material back to the posterior rim of the vertebral body. Once the disc space is meticulously prepared, a properly sized implant, consisting of plates that fit the vertebral endplates and a polyethylene spacer that permits a limited degree of motion, is inserted and carefully embedded into the bone
Once the wound is closed, the patient is mobilized immediately; as there is no fusion desired, the patient can be up and about and moving right after surgery. Results to date have been very encouraging. Long term results can only be estimated, however, since these implants are new to general use.
Spinal Instrumentation
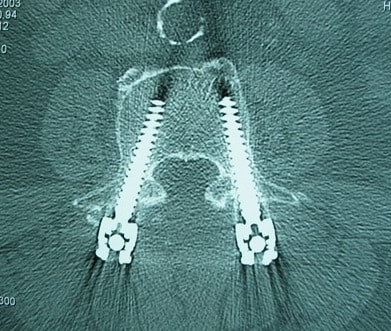
In the realm of spinal fusion, spinal instrumentation serves three purposes: 1) it reduces or eliminates the need for external bracing 2) it improves the likelihood of successful fusion 3) it minimizes the number of spinal motion segments that need to be fused.
Patients who have instrumentation can be started on more aggressive post-operative rehabilitation and are more easily mobilized. Addition of rigid instrumentation has also been shown to increase fusion rates in degenerative disease with little increased risk of complications.
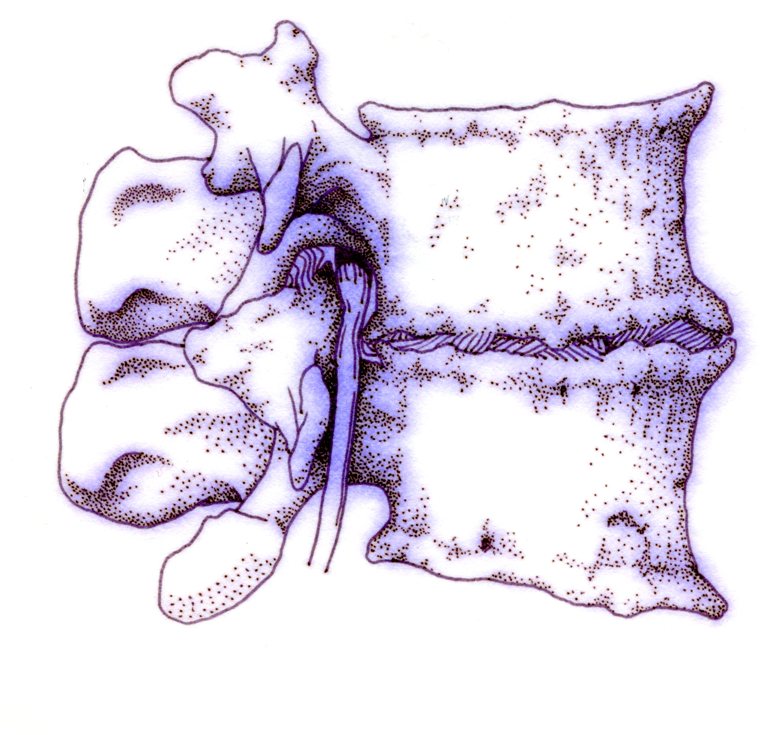
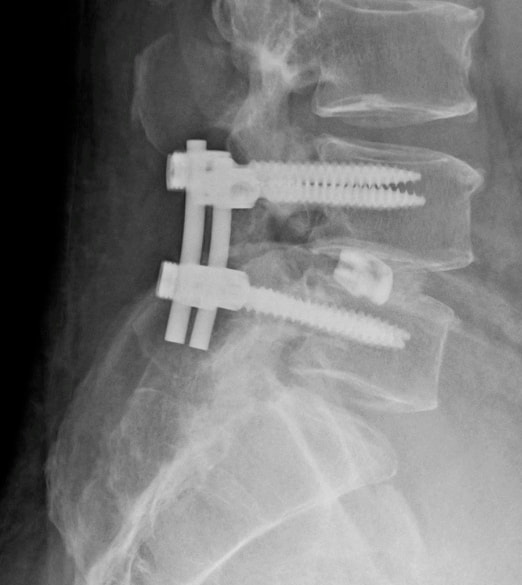
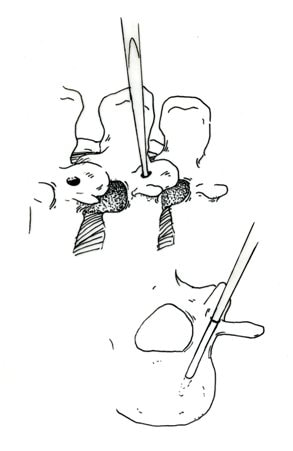
Posterior instrumentation consists primarily of pedicle screws and connecting rods. The pedicle screws are inserted in a very precise manner, entering the vertebral posterior elements at the junction of the transverse process and the inferior rim of the upper facet, and traveling through the interior of the vertebral pedicle into the vertebral body. Placed correctly, the screw is entirely contained inside the bone, and provides strong fixation to the vertebral body.
Spinal Instrumentation
In the realm of spinal fusion, spinal instrumentation serves three purposes: 1) it reduces or eliminates the need for external bracing 2) it improves the likelihood of successful fusion 3) it minimizes the number of spinal motion segments that need to be fused.
Patients who have instrumentation can be started on more aggressive post-operative rehabilitation and are more easily mobilized. Addition of rigid instrumentation has also been shown to increase fusion rates in degenerative disease with little increased risk of complications.
Posterior instrumentation consists primarily of pedicle screws and connecting rods. The pedicle screws are inserted in a very precise manner, entering the vertebral posterior elements at the junction of the transverse process and the inferior rim of the upper facet, and traveling through the interior of the vertebral pedicle into the vertebral body. Placed correctly, the screw is entirely contained inside the bone, and provides strong fixation to the vertebral body.
Screws placed in adjacent vertebrae are then connected with longitudinal rods, providing an internal splint far more effective than any external brace or cast.
Pedicle Screws:
Pedicle screws and rods are used to insure successful posterolateral fusion, and to reduce the number of motion segments that must be fused. They are placed through the junction of the transverse process and facet, traveling through the inside of the pedicle and into the vertebral body. Pedicle screws have been used in Europe for more than 40 years and have been shown to be safe and effective when properly and carefully inserted. Computer assisted navigation and fluoroscopy help limit the risk of a screw being placed in poor alignment, and some surgeons now employ robotic systems to help place the screws accurately and consistently.
Pedicle Screws:
Pedicle screws and rods are used to insure successful posterolateral fusion, and to reduce the number of motion segments that must be fused. They are placed through the junction of the transverse process and facet, traveling through the inside of the pedicle and into the vertebral body. Pedicle screws have been used in Europe for more than 40 years and have been shown to be safe and effective when properly and carefully inserted. Computer assisted navigation and fluoroscopy help limit the risk of a screw being placed in poor alignment, and some surgeons now employ robotic systems to help place the screws accurately and consistently.
The screws selected are picked according to the size and depth of each vertebral pedicle - the bone that connects the vertebral body in front to the lamina and facet joint in the back. Screws can be placed "free-hand" with the surgeon creating a starting hole and passing a probe down the pedicle under fluoroscopic control, or under image guidance where the landmarks for starting and finishing screw placement are determined from an imaging system with computer guidance built into the probes and drill systems.
Most surgeons use a blunt tipped probe to minimize the chance of perforating the pedicle wall as the pilot hole for the screw is created, and then use a ball-tipped probe to directly feel the wall of the pedicle to confirm integrity.
Most surgeons use a blunt tipped probe to minimize the chance of perforating the pedicle wall as the pilot hole for the screw is created, and then use a ball-tipped probe to directly feel the wall of the pedicle to confirm integrity.
If the bone is intact all around the screw hole, the screw can be placed with excellent safety. The position of the screw is then double-checked on x-ray or fluoroscopy.
With the screws in place the bone graft is applied over the transverse processes and the screws are connected by rods to provide the internal splint that will help the fusion to heal. Most contemporary systems used in the spine are made from titanium, which heals in well with the surrounding bone, is easier to image around, and does not contain any of the metals that can cause metal allergies or "metallosis".
Interbody Cages
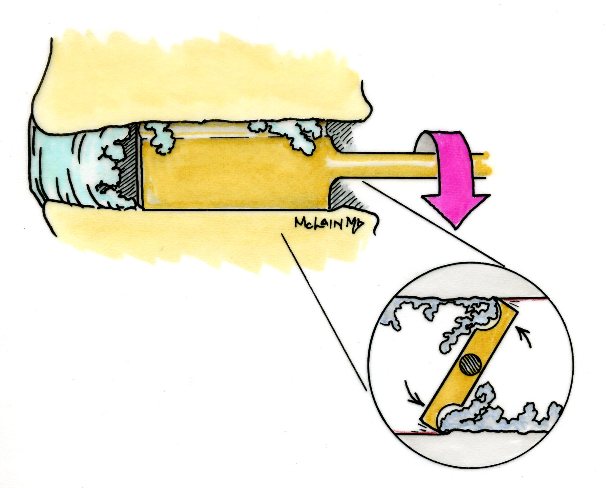
Along with pedicle screw placement, the surgeon may elect to perform an interbody fusion using either an ALIF or TLIF approach.
The TLIF is carried out at the time of pedicle screw placement, and requires a laminectomy, which is often already needed to allow discectomy or removal of bone spurs to take pressure off of the nerve roots. Beginning in an anatomic “safe zone” between the nerve root and the thecal sac, the surgeon removes disc material to complete a full discectomy. The surgeon then inserts a series of blunt paddles that distract the disc space, restoring the disc space height, correcting sagittal alignment, and creating a space for the fusion cage that is placed next.
With the screws in place the bone graft is applied over the transverse processes and the screws are connected by rods to provide the internal splint that will help the fusion to heal. Most contemporary systems used in the spine are made from titanium, which heals in well with the surrounding bone, is easier to image around, and does not contain any of the metals that can cause metal allergies or "metallosis".
Interbody Cages
Along with pedicle screw placement, the surgeon may elect to perform an interbody fusion using either an ALIF or TLIF approach.
The TLIF is carried out at the time of pedicle screw placement, and requires a laminectomy, which is often already needed to allow discectomy or removal of bone spurs to take pressure off of the nerve roots. Beginning in an anatomic “safe zone” between the nerve root and the thecal sac, the surgeon removes disc material to complete a full discectomy. The surgeon then inserts a series of blunt paddles that distract the disc space, restoring the disc space height, correcting sagittal alignment, and creating a space for the fusion cage that is placed next.
Once maximal distraction has occurred, the pedicle screw fixation nuts are tightened on the working rods to hold the space open.
The surgeon now removes all of the end-plate cartilage from the vertebra on each side of the disc space, and exposes a large surface of bone for fusion. If too much endplate bone is removed, the interbody cages are more likely to sink into the softer cancellous bone.
The surgeon now removes all of the end-plate cartilage from the vertebra on each side of the disc space, and exposes a large surface of bone for fusion. If too much endplate bone is removed, the interbody cages are more likely to sink into the softer cancellous bone.
The prepared interspace is then filled with bone graft material, and an interbody spacer.
There are several options for an interbody cage but most cages used now are made of PEEK - a plastic like material that is well tolerated by bone and easy to x-ray through, or titanium, which can be made with a microsurface that bone actually grows into.
There are several options for an interbody cage but most cages used now are made of PEEK - a plastic like material that is well tolerated by bone and easy to x-ray through, or titanium, which can be made with a microsurface that bone actually grows into.
While the goals and fundamental principles are the same for each of the different types of spacer, the application techniques, and the nuances of their use do vary. This is particularly true of MIS techniques that may include quite unique interbody spacers.
When used in combination with appropriate posterior instrumentation, these cages provide excellent initial stability, allow correction of deformities, and provide a high rate of fusion success. Radiolucent devices permit us to accurately assess how the graft incorporates and see the interbody fusion. Successful cage placement and solid fusion requires meticulous preparation of the interspace and endplates, however.
Before placing the cages, morselized bone graft is packed into the anterior interspace to densely fill that portion of the disc space. The cage, packed with autograft morsels, is introduced and impacted into place. The distraction force is released, and the pedicle screws are compressed towards each other to capture the cages and restore lordosis.
Things We Worry About During Spinal Surgery
Regardless of surgical strategy or operative approach, complications can occur with any surgical procedure. Surgeons work hard to prevent as many complications as they can and to anticipate and minimize those that they can’t prevent.
Intraoperative complications can arise from problems with the instrumentation whether it is placed correctly or not. Injuries to vascular or visceral structures are very rare with pedicle screw fixation, but misplaced pedicle screws may occur in up to 5% of patients. Many of these screws will cause no problem, work satisfactorily, and not require revision. Misplacement occurs more frequently in scoliosis and with more inexperienced surgeons and can occasionally injure or irritate a nerve root, requiring another surgery.
Permanent neurological injury is the most feared complication in spinal surgery. The rate of injury associated with instrumented lumbar fusions has been seen to be slightly higher than in un-instrumented fusions, but in experienced hands both rates are very low. Most nerve irritation comes from moving the nerve around during decompression or removal of scar. When nerve monitoring in the operating room shows that nerve signals have changed during placement of a screw, prompt removal of that screw is indicated. Nerve or spinal cord injury can be related to pressure on the tissue itself, or damage from a probe or instrument, but can also occur if the patient's blood pressure drops for an extended period. For this reason spine surgery is often carried out by anesthesiologists with extensive spine experience.
Injury to the neural tissues may not always injure the nerves, but a tear in the covering (dura) that protects the nerves can be a big problem during surgery as well. Dural tears result in cerebrospinal fluid leaks, which can occur during decompressive procedures performed to treat nerve compression, require a microsurgical repair with very fine suture to prevent persistent fluid leaks and post-operative headaches
When used in combination with appropriate posterior instrumentation, these cages provide excellent initial stability, allow correction of deformities, and provide a high rate of fusion success. Radiolucent devices permit us to accurately assess how the graft incorporates and see the interbody fusion. Successful cage placement and solid fusion requires meticulous preparation of the interspace and endplates, however.
Before placing the cages, morselized bone graft is packed into the anterior interspace to densely fill that portion of the disc space. The cage, packed with autograft morsels, is introduced and impacted into place. The distraction force is released, and the pedicle screws are compressed towards each other to capture the cages and restore lordosis.
Things We Worry About During Spinal Surgery
Regardless of surgical strategy or operative approach, complications can occur with any surgical procedure. Surgeons work hard to prevent as many complications as they can and to anticipate and minimize those that they can’t prevent.
Intraoperative complications can arise from problems with the instrumentation whether it is placed correctly or not. Injuries to vascular or visceral structures are very rare with pedicle screw fixation, but misplaced pedicle screws may occur in up to 5% of patients. Many of these screws will cause no problem, work satisfactorily, and not require revision. Misplacement occurs more frequently in scoliosis and with more inexperienced surgeons and can occasionally injure or irritate a nerve root, requiring another surgery.
Permanent neurological injury is the most feared complication in spinal surgery. The rate of injury associated with instrumented lumbar fusions has been seen to be slightly higher than in un-instrumented fusions, but in experienced hands both rates are very low. Most nerve irritation comes from moving the nerve around during decompression or removal of scar. When nerve monitoring in the operating room shows that nerve signals have changed during placement of a screw, prompt removal of that screw is indicated. Nerve or spinal cord injury can be related to pressure on the tissue itself, or damage from a probe or instrument, but can also occur if the patient's blood pressure drops for an extended period. For this reason spine surgery is often carried out by anesthesiologists with extensive spine experience.
Injury to the neural tissues may not always injure the nerves, but a tear in the covering (dura) that protects the nerves can be a big problem during surgery as well. Dural tears result in cerebrospinal fluid leaks, which can occur during decompressive procedures performed to treat nerve compression, require a microsurgical repair with very fine suture to prevent persistent fluid leaks and post-operative headaches
Dural tears, or durotomies, are significantly more likely during revision surgery. Patients suffering a dural tear will have a longer surgery, as the tear is typically repaired using an operating microscope. They will also spend a little more time in bed after surgery, to let the tear seal before standing up. If the leak persists, the patient may experience headaches, similar to "myelogram headaches", necessitating further treatment to seal the tear.
Finally, the most common complication, and a serious complication in any patient, is infection. Patients undergoing any kind of procedure that breaks the skin - even an injection - have a risk of getting an infection. And the usual bacterial agents that cause infection are the ones we can't get completely away from...the ones that live on our own skin. All the preoperative methods we use to sterilize the incision site, our instruments, and our gown and gloves greatly reduces the risk of infection, but that risk is never down to zero.
So we take several precautions to reduce that risk as low as we can. It is routine nowadays (standard of care) for Orthopaedic patients to receive a dose of appropriate antibiotics, by IV, prior to the start of surgery, and if the surgery is long or complex, they may get additional doses.
Many surgeons will add to antibiotic coverage by washing the wound with an antibiotic solution prior to closure, and others will apply an antibiotic medication into the depths of the wound itself. Proper post-operative wound care keeps the wound clean and safe until the skin has a chance to seal and protect itself.
Still, there is a measurable rate of superficial wound infections that require examination and oral antibiotics, and a small but never "zero" number of patients that develop a deep infection that requires re-operation and hospitalization, along with long-term antibiotics, no matter what strategy is used. Patients with excess body weight, diabetes, impaired immunity, smokers, and those undergoing revision of older surgeries are all at increased risk.
Post-operative Care and Activities
Patients undergoing posterior instrumentation for degenerative disorders, spondylolisthesis, or discogenic pain, are really quite stable after surgery and need only a corset for comfort after their operation. Those with more post-operative instability, due to removal of a tumor or treatment of a fracture, may benefit from external bracing, such as a thoracolumbosacral orthosis, (TLSO). Depending on the number of levels treated, the extent of blood loss, and the patient's baseline health, hospitalization and physical therapy may be needed, but many single level and minimally invasive spinal fusions can be carried out as outpatient surgeries, with patients up at bedside an hour after anesthesia and home later the same day.
Patients who have undergone more extensive or anterior/posterior surgeries will generally be fully ambulatory within 2-3 days postoperatively unless neurologic problems or other medical problems exist that interfere. The patient can expect "surgical" pain for approximately 5 to 7 days after surgery, and some pain for up to 6 weeks should be expected as muscles recover from the injury of the operation.
Patients with a stable spine, and those with a combined anterior and posterior reconstruction wear their brace to protect muscles during the early healing phase, but can be up without it with little fear of problems. These patients can advance activities as tolerated, can bend to put their socks and shoes on, and can begin lifting and carrying limited loads within a week of surgery. They may discontinue the brace after 4 – 6 weeks, but often find the support helpful when increasing activities thereafter. They can start back to light duty work at three to six weeks from surgery, and should be back to full duty or to active physical therapy by 12 weeks. Patients with spinal instability or poor bone quality may need to wear their TLSO for up to 4 months, and will also be fitted with a bone stimulator that aids the bone formation process.
Patients may ambulate to tolerance and are encouraged to walk up to 2 miles per day. Riding in a car is fine, but driving is not recommended for approximately 4-6 weeks. Heavy lifting (objects over 15 pounds) should be avoided for the first 6 weeks. At 6 weeks, bicycle or treadmill activity may be added to the physical therapy program, as well as increased walking and stair climbing. Work hardening, depending on job classification, is begun at 12 to 24 weeks. Light‑duty work activities are begun at 3 - 6 weeks and heavy‑duty, unrestricted activities at 3 - 6 months depending on the patient and the job.
The surgical implants (screws and rods or plates) are only necessary during the fusion period. Once the spine is fused these devices become more or less redundant. Currently, surgeons rarely remove the implants unless the components are prominent under the skin or have become loose in the face of a failed fusion.
Conclusion
Surgical care for back pain is more about the correction of instability, deformity, disc disruption, or decompression of nerve elements, and less about "fixing pain". If the basic problem is one of the above, then the pain is very likely to improve or resolve when the underlying problem is fixed.
Spine surgeons go to lengths (sometimes frustrating lengths) to make sure your pain is coming from a correctable, treatable cause, and then to plan the operation that will eliminate that problem and the pain safely and reliably.
Finally, the most common complication, and a serious complication in any patient, is infection. Patients undergoing any kind of procedure that breaks the skin - even an injection - have a risk of getting an infection. And the usual bacterial agents that cause infection are the ones we can't get completely away from...the ones that live on our own skin. All the preoperative methods we use to sterilize the incision site, our instruments, and our gown and gloves greatly reduces the risk of infection, but that risk is never down to zero.
So we take several precautions to reduce that risk as low as we can. It is routine nowadays (standard of care) for Orthopaedic patients to receive a dose of appropriate antibiotics, by IV, prior to the start of surgery, and if the surgery is long or complex, they may get additional doses.
Many surgeons will add to antibiotic coverage by washing the wound with an antibiotic solution prior to closure, and others will apply an antibiotic medication into the depths of the wound itself. Proper post-operative wound care keeps the wound clean and safe until the skin has a chance to seal and protect itself.
Still, there is a measurable rate of superficial wound infections that require examination and oral antibiotics, and a small but never "zero" number of patients that develop a deep infection that requires re-operation and hospitalization, along with long-term antibiotics, no matter what strategy is used. Patients with excess body weight, diabetes, impaired immunity, smokers, and those undergoing revision of older surgeries are all at increased risk.
Post-operative Care and Activities
Patients undergoing posterior instrumentation for degenerative disorders, spondylolisthesis, or discogenic pain, are really quite stable after surgery and need only a corset for comfort after their operation. Those with more post-operative instability, due to removal of a tumor or treatment of a fracture, may benefit from external bracing, such as a thoracolumbosacral orthosis, (TLSO). Depending on the number of levels treated, the extent of blood loss, and the patient's baseline health, hospitalization and physical therapy may be needed, but many single level and minimally invasive spinal fusions can be carried out as outpatient surgeries, with patients up at bedside an hour after anesthesia and home later the same day.
Patients who have undergone more extensive or anterior/posterior surgeries will generally be fully ambulatory within 2-3 days postoperatively unless neurologic problems or other medical problems exist that interfere. The patient can expect "surgical" pain for approximately 5 to 7 days after surgery, and some pain for up to 6 weeks should be expected as muscles recover from the injury of the operation.
Patients with a stable spine, and those with a combined anterior and posterior reconstruction wear their brace to protect muscles during the early healing phase, but can be up without it with little fear of problems. These patients can advance activities as tolerated, can bend to put their socks and shoes on, and can begin lifting and carrying limited loads within a week of surgery. They may discontinue the brace after 4 – 6 weeks, but often find the support helpful when increasing activities thereafter. They can start back to light duty work at three to six weeks from surgery, and should be back to full duty or to active physical therapy by 12 weeks. Patients with spinal instability or poor bone quality may need to wear their TLSO for up to 4 months, and will also be fitted with a bone stimulator that aids the bone formation process.
Patients may ambulate to tolerance and are encouraged to walk up to 2 miles per day. Riding in a car is fine, but driving is not recommended for approximately 4-6 weeks. Heavy lifting (objects over 15 pounds) should be avoided for the first 6 weeks. At 6 weeks, bicycle or treadmill activity may be added to the physical therapy program, as well as increased walking and stair climbing. Work hardening, depending on job classification, is begun at 12 to 24 weeks. Light‑duty work activities are begun at 3 - 6 weeks and heavy‑duty, unrestricted activities at 3 - 6 months depending on the patient and the job.
The surgical implants (screws and rods or plates) are only necessary during the fusion period. Once the spine is fused these devices become more or less redundant. Currently, surgeons rarely remove the implants unless the components are prominent under the skin or have become loose in the face of a failed fusion.
Conclusion
Surgical care for back pain is more about the correction of instability, deformity, disc disruption, or decompression of nerve elements, and less about "fixing pain". If the basic problem is one of the above, then the pain is very likely to improve or resolve when the underlying problem is fixed.
Spine surgeons go to lengths (sometimes frustrating lengths) to make sure your pain is coming from a correctable, treatable cause, and then to plan the operation that will eliminate that problem and the pain safely and reliably.
Understanding your diagnosis, and what the goals of surgical treatment are, as well as understanding what recovery and rehabilitation will entail, will help you make good decisions and get good results if you have a back pain problem that requires spinal surgery.